Vision for a Lifetime
No matter what your age, if you’re dreaming of seeing life in clear, vibrant color with more freedom from glasses, contacts, and even reading glasses, we’ve got a vision correction solution for you!

Age 18 - 44
Age 18 - 44
Tired of the hassles of glasses and contacts? Ocala Eye can help you reclaim visual freedom to do what you love most without corrective lenses with LASIK.

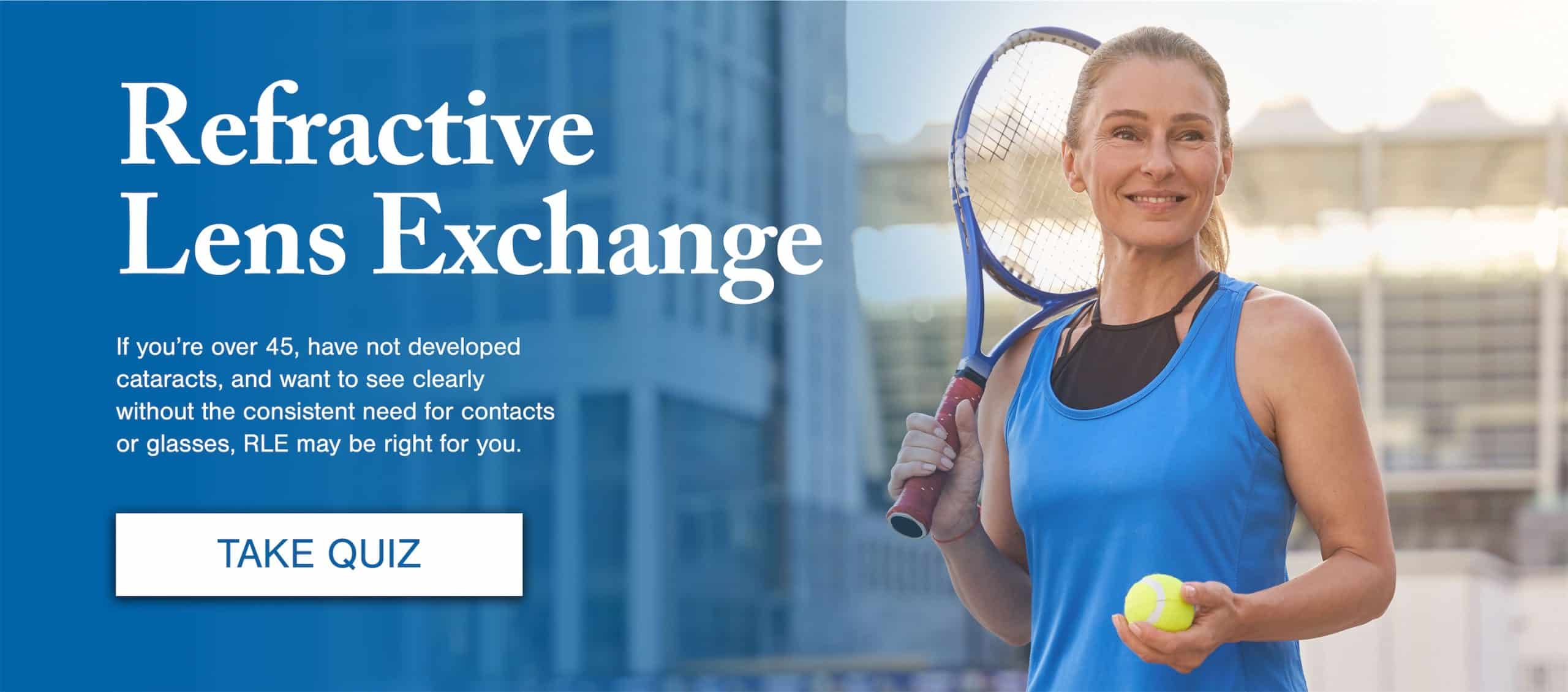
Age 45 - 60
Age 45 - 60
RLE (Refractive Lens Exchange) is a popular option for those over the age of 45 who could never have dreamed of being free from glasses, contacts, and even reading glasses.
Age 60+
Age 60+
We offer advanced cataract surgery that can help you see clearly in the distance, up close, and everything in between with less dependence on glasses, contacts, and reading glasses.
North Central Florida’s Best Reviewed Eyecare Provider
Ocala Eye is the largest, most experienced eye care practice in North Central Florida. Since Ocala Eye was founded in 1971, more people from The Villages, Marion and surrounding counties trust their eyes to our ophthalmologists than any other eye care group.
We are a patient-centered practice, with all of the decisions made based on the patient’s benefit and well-being. This philosophy is reflected by our patients’ satisfaction and our passion for providing complete eye care and aesthetic services.